Appendix diverticula is uncommon and a strong marker for appendiceal neoplasm. Signs and symptoms are unlikely to be different from appendicitis and the diagnosis is usually made on histological analysis rather than at surgery.
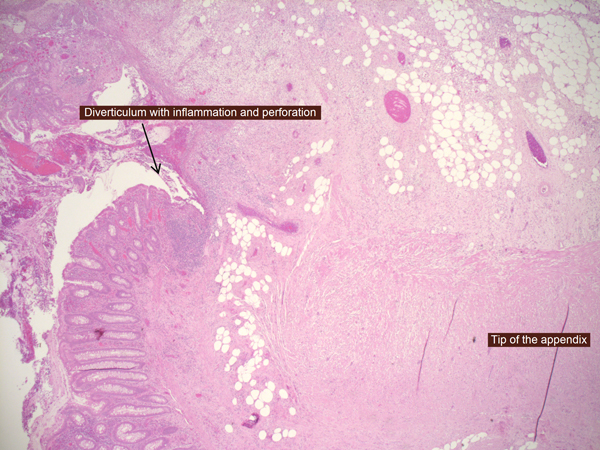 Case report: This is a case report of a 54- years old gentleman who presented to the Surgical Emergency Unit (SEU) with a 3 days history of cramping peri-umbilical abdominal pain radiating to the right iliac fossa (RIF) worse on movement and coughing. He felt nauseated and had lost his appetite. He also complained about loose stools without blood or mucous. There were no symptoms or evidence of lower urinary tract infection. Past medical history comprised Chronic Obstructive Pulmonary Disease (COPD) for which he was on Salbutamol inhalers. He had not undergone previous surgery. On examination he had a temperature of 37.3 ºC, pulse 94 beats per minute and blood pressure 118/76. The abdomen was tense with guarding and rebound tenderness present in RIF. Admission leucocyte, neutrophil counts and C-reactive protein were 12.0, 10.0 x 109/l and 325 mg/l respectively. An abdominal ultrasound revealed a mixed echogenic area measuring 5 x 2 cm within the RIF raising the possibility of a collection. Intravenous antibiotics were commenced. At diagnostic laparoscopy, small bowel and omentum were adherent to a pus-filled inflamed appendix. A standard laparoscopic appendicectomy was performed. Postoperative recovery was uneventful, and patient was discharged on day 4. Histology revealed Appendix Diverticulitis (AD) and no malignancy was identified. ( figure 1) Discussion: Appendicular diverticulum (AD) has a reported incidence of 0.004 – 2.1 % [1]. It can be associated with significant pathology such as neoplasm, perforation and gastrointestinal (GI) bleeding. The pathogenesis for GI bleeding from an AD is unclear but should be considered in the differential diagnosis of GI bleed particularly in the young age group [2]. Treatment in the form of appendicectomy produces a good outcome. As the association between AD and appendix neoplasm is strong, a colonoscopy is recommended if such a lesion is not found in the appendix remnant. Ultrasound can help in the diagnosis of AD in 33 % of cases [3], In our patient, ultrasound had revealed a mixed echogenic area in the right iliac fossa representative of peri-appendiceal loculated fluid. Conclusion: Diverticulum of the appendix is likely to be associated with an appendix neoplasm. AD and acute appendicitis cannot be clearly differentiated on clinical symptoms and signs. Imaging maybe be helpful in diagnosis as in our patient it revealed an echogenic mass. These patients are treated with an appendicectomy and a postoperative colonoscopy is offered if the appendix is clear of tumour/growths on histology. Figure 1: Appendix Diverticulitis with Perforation. The appendix diverticulum is located at the tip of the appendix References 1. Kabiri H, Clarke LE, Tzarnas CD. Appendiceal diverticulitis. Am Surg [Internet]. 2006 Mar;72(3):221–3. 2. Ogawa Y, Asayama N, Nagata S. Acute gastrointestinal bleeding from appendiceal diverticulitis diagnosed preoperatively by combined short-interval computed tomography and colonoscopy: A case report. Dig Endosc [Internet]. 2018 May;30(3):392–4. 3. Yamana I, Kawamoto S, Inada K, Nagao S, Yoshida T, Yamashita Y. Clinical characteristics of 12 cases of appendiceal diverticulitis: a comparison with 378 cases of acute appendicitis. Surg Today [Internet]. 2012 Apr;42(4):363–7.
Case report: This is a case report of a 54- years old gentleman who presented to the Surgical Emergency Unit (SEU) with a 3 days history of cramping peri-umbilical abdominal pain radiating to the right iliac fossa (RIF) worse on movement and coughing. He felt nauseated and had lost his appetite. He also complained about loose stools without blood or mucous. There were no symptoms or evidence of lower urinary tract infection. Past medical history comprised Chronic Obstructive Pulmonary Disease (COPD) for which he was on Salbutamol inhalers. He had not undergone previous surgery. On examination he had a temperature of 37.3 ºC, pulse 94 beats per minute and blood pressure 118/76. The abdomen was tense with guarding and rebound tenderness present in RIF. Admission leucocyte, neutrophil counts and C-reactive protein were 12.0, 10.0 x 109/l and 325 mg/l respectively. An abdominal ultrasound revealed a mixed echogenic area measuring 5 x 2 cm within the RIF raising the possibility of a collection. Intravenous antibiotics were commenced. At diagnostic laparoscopy, small bowel and omentum were adherent to a pus-filled inflamed appendix. A standard laparoscopic appendicectomy was performed. Postoperative recovery was uneventful, and patient was discharged on day 4. Histology revealed Appendix Diverticulitis (AD) and no malignancy was identified. ( figure 1) Discussion: Appendicular diverticulum (AD) has a reported incidence of 0.004 – 2.1 % [1]. It can be associated with significant pathology such as neoplasm, perforation and gastrointestinal (GI) bleeding. The pathogenesis for GI bleeding from an AD is unclear but should be considered in the differential diagnosis of GI bleed particularly in the young age group [2]. Treatment in the form of appendicectomy produces a good outcome. As the association between AD and appendix neoplasm is strong, a colonoscopy is recommended if such a lesion is not found in the appendix remnant. Ultrasound can help in the diagnosis of AD in 33 % of cases [3], In our patient, ultrasound had revealed a mixed echogenic area in the right iliac fossa representative of peri-appendiceal loculated fluid. Conclusion: Diverticulum of the appendix is likely to be associated with an appendix neoplasm. AD and acute appendicitis cannot be clearly differentiated on clinical symptoms and signs. Imaging maybe be helpful in diagnosis as in our patient it revealed an echogenic mass. These patients are treated with an appendicectomy and a postoperative colonoscopy is offered if the appendix is clear of tumour/growths on histology. Figure 1: Appendix Diverticulitis with Perforation. The appendix diverticulum is located at the tip of the appendix References 1. Kabiri H, Clarke LE, Tzarnas CD. Appendiceal diverticulitis. Am Surg [Internet]. 2006 Mar;72(3):221–3. 2. Ogawa Y, Asayama N, Nagata S. Acute gastrointestinal bleeding from appendiceal diverticulitis diagnosed preoperatively by combined short-interval computed tomography and colonoscopy: A case report. Dig Endosc [Internet]. 2018 May;30(3):392–4. 3. Yamana I, Kawamoto S, Inada K, Nagao S, Yoshida T, Yamashita Y. Clinical characteristics of 12 cases of appendiceal diverticulitis: a comparison with 378 cases of acute appendicitis. Surg Today [Internet]. 2012 Apr;42(4):363–7.